Scientists have discovered that a common type of bacteria that causes infections in hospitals can break down biodegradable plastics that are often used in medical devices and packaging.
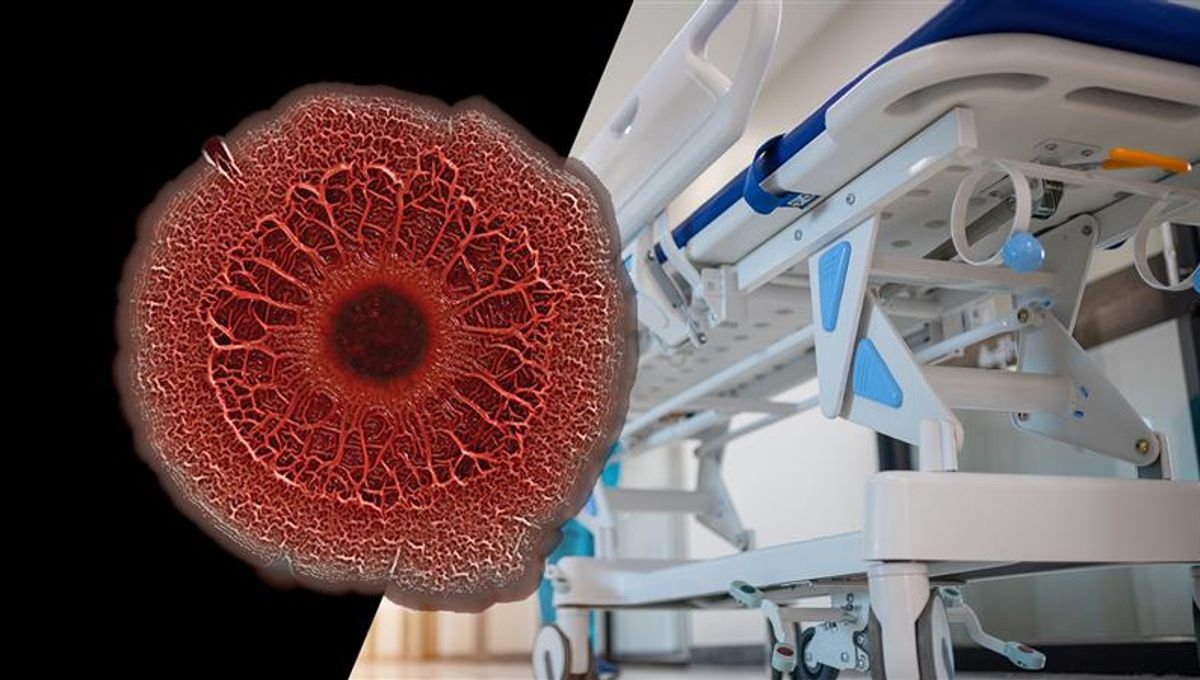
The bacterium in question, known as Pseudomonas aeruginosa, is a gram-negative (a classification based on the color the bacterium turns after it has undergone a Gram staining test), rod-shaped bacterial species, and is adaptable and extremely opportunistic, especially in clinical settings. It is a common cause of hospital infections, causing problems such as pneumonia, urinary tract infections, and sepsis, among other issues.
The bacterium is also pretty tough. Some types are resistant to nearly all antibiotics (known as multidrug-resistant, or MDR P. aeruginosa), hence it is often dubbed a “superbug“. In the US, this strain is known to cause thousands of deaths in hospitalized patients each year, as well as tens of thousands of non-lethal infections. Those with weakened immune systems are particularly vulnerable to such infections.
It’s a troublesome organism, but now researchers have found that it is capable of breaking down plastics commonly used in hospitals.
Carried out in the United Kingdom, this research identified an enzyme, named Pap1, that was produced by P. aeruginosa taken from a wound. This enzyme can break down biodegradable plastic called polycaprolactone (PCL), which is used in various medical packages and devices, such as sutures, catheters, ventilators, implants, and plastic packaging for medical tools.
To date, multiple bacteria have been found to produce enzymes that degrade plastic, but they have all been isolated from the environment. This is the first time one has been identified in a clinical setting.
It’s an important development, as it could explain why these bacteria are so persistent in hospitals. If they’re able to degrade plastic, then they may be able to contaminate surfaces and tools that are otherwise thought to be sterile.
In order to identify this enzyme, the researchers took the gene that codes for the enzyme and transplanted it into Escherichia coli bacteria. When E. coli expressed this enzyme, the team found that it started to break down the PCL on agar plates or beads. The same was true for the P. aeruginosa isolated from the wound. Finally, the team produced a P. aeruginosa bacterium that had the gene encoding Pap1 removed from it; they found that this version was not capable of degrading plastics.
“This poses several clinical challenges with respect to infection. PCL is widely used in medical care and is one of the materials at the forefront of biotechnological innovation due to its favorable biocompatibility profile,” the team explains in their paper.
“From a host perspective, the capacity for a pathogen to be able to compromise the structural integrity of any medical device or implant that contains PCL is likely to cause the failure of the medical intervention.”
It is possible that this ability to degrade plastic helps the bacteria survive. If they can create small pits or impressions in the plastic, they have a chance to use them as niches that shield the bacteria from the immune system, disinfectants, or antibiotics.
The team also found that the enzyme increases the amount of biofilm the bacteria can produce when compared to a different surface, such as glass. Generally speaking, if bacteria produce higher amounts of biofilm, they are more likely to be resistant to antibiotics.
“Biofilms are the dominant mode of growth for bacteria, and adopting this mode of growth can make pathogens particularly recalcitrant to treatment,” the team explains.
In order to test whether the ability of these bacteria to form biofilms would make them more virulent, the team also implanted them into greater wax moth (Galleria mellonella) larvae. They found that changing the presence of the enzyme-producing gene in the P. aeruginosa implant impacted the larvae’s survivability; bacteria that lacked the PCL implant were less harmful than those that had it present.
Ultimately, the results demonstrate the risks P. aeruginosa poses in medical settings, as it can increase infection rates and also degrade medical plastics.
“As it can be degraded by the causative agent of an infection, the potential for increased infection risk and even accelerated degradation of implants or sutures should be considered in device design and treatment planning,” they note.
“Antimicrobial components could be added to PCL medical devices to reduce the risk of infection and biodegradation.”
The team is now developing tests to check whether other pathogens can produce plastic-degrading enzymes.
The study is published in Cell Reports.
Source Link: For The First Time, Common Hospital “Superbug” Found To Break Down Medical Plastics