A new biomarker that can be used to identify neurodegeneration associated with Alzheimer’s disease in the blood has been identified. The discovery could one day lead to a diagnostic blood test for the disease, eliminating the need for invasive and costly procedures.
As senior study author Thomas Karikari of the University of Pittsburgh said in a statement: “At present, diagnosing Alzheimer’s disease requires neuroimaging. Those tests are expensive and take a long time to schedule, and…accessibility is a major issue.”
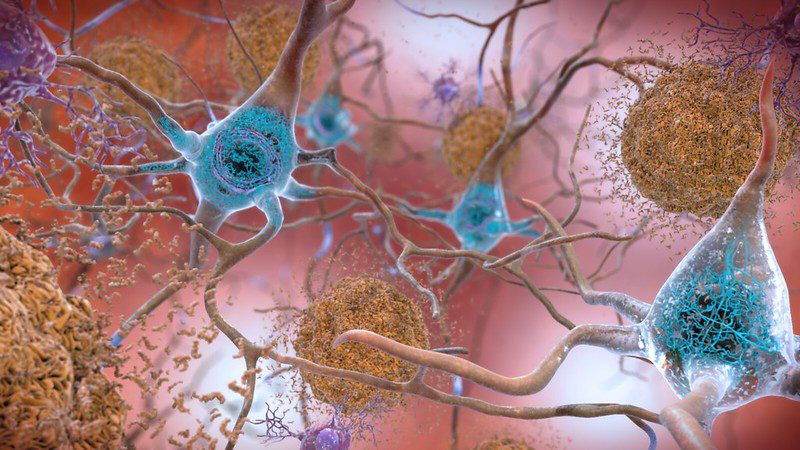
Current guidelines require clinicians to detect three distinct features of Alzheimer’s in the patient’s brain before a diagnosis can be made: plaques of amyloid-β protein; tau protein tangles; and evidence of neurodegeneration. The usual way to identify these features is to use magnetic resonance imaging (MRI) or positron emission tomography (PET) scans, or to analyze samples of cerebrospinal fluid obtained via lumbar puncture (sometimes known as a spinal tap).
MRI and PET scans are expensive, time-consuming to arrange, and simply not accessible to everyone. Lumbar punctures, meanwhile, can be painful and cause side effects such as a long-lasting headache. Because of these limitations, the team behind the new study sought to come up with a minimally invasive approach that could reliably diagnose Alzheimer’s disease with less demand on resources.
And it seems that they have found it in “brain-derived tau”, or BD-tau.
Blood tests for Alzheimer’s are not a new idea, but so far they have struggled to overcome one particular hurdle. It’s possible to accurately detect abnormal amyloid protein in blood plasma, as well as phosphorylated tau protein – that’s two checkmarks against the list of three clinical features that are needed to confidently diagnose Alzheimer’s. But, there remains the problem of neurodegeneration.
The best biomarker of neurodegeneration we can currently detect in blood plasma is called neurofilament light chain (NfL). However, as the study authors point out, NfL “is unable to differentiate between Alzheimer’s disease and other dementias due to its increases in a wide range of neurodegenerative disorders. Consequently, the dementia research field currently lacks a blood biomarker that is specifically altered as a result of Alzheimer-type neurodegenerative changes.”
Seeking a diagnostic test with greater specificity, the team developed an antibody that selectively binds to BD-tau, while avoiding the so-called “big tau” proteins that are produced by cells outside the brain. Validation of the new antibody test in over 600 patient samples showed that it was effective at diagnosing Alzheimer’s disease, and – crucially – at distinguishing Alzheimer’s from other neurodegenerative conditions.
If larger-scale validation goes well, and the BD-tau test is shown to be effective in people from all backgrounds and at different disease stages, it could become a cheaper and more accessible way of diagnosing Alzheimer’s. Not only that – the team hope that having this test at our disposal could lead to improvements in clinical trial design.
“There is a huge need for diversity in clinical research, not just by skin color but also by socioeconomic background,” said Karikari. “To develop better drugs, trials need to enroll people from varied backgrounds and not just those who live close to academic medical centers.”
“A blood test is cheaper, safer and easier to administer, and it can improve clinical confidence in diagnosing Alzheimer’s and selecting participants for clinical trial and disease monitoring.”
The study is published in the journal Brain.
Source Link: New Blood Test Could Spot Alzheimer’s Disease Without The Need For Expensive Scans