A common treatment strategy in patients with liver disease may be inadvertently leading Enterococcus faecium bacteria to develop resistance to one of the last effective antibiotics we have, according to a new preprint. The research, which is yet to be peer-reviewed, found that treating patients with rifaximin was associated with genetic mutations in E. faecium that confer resistance to the antibiotic daptomycin.
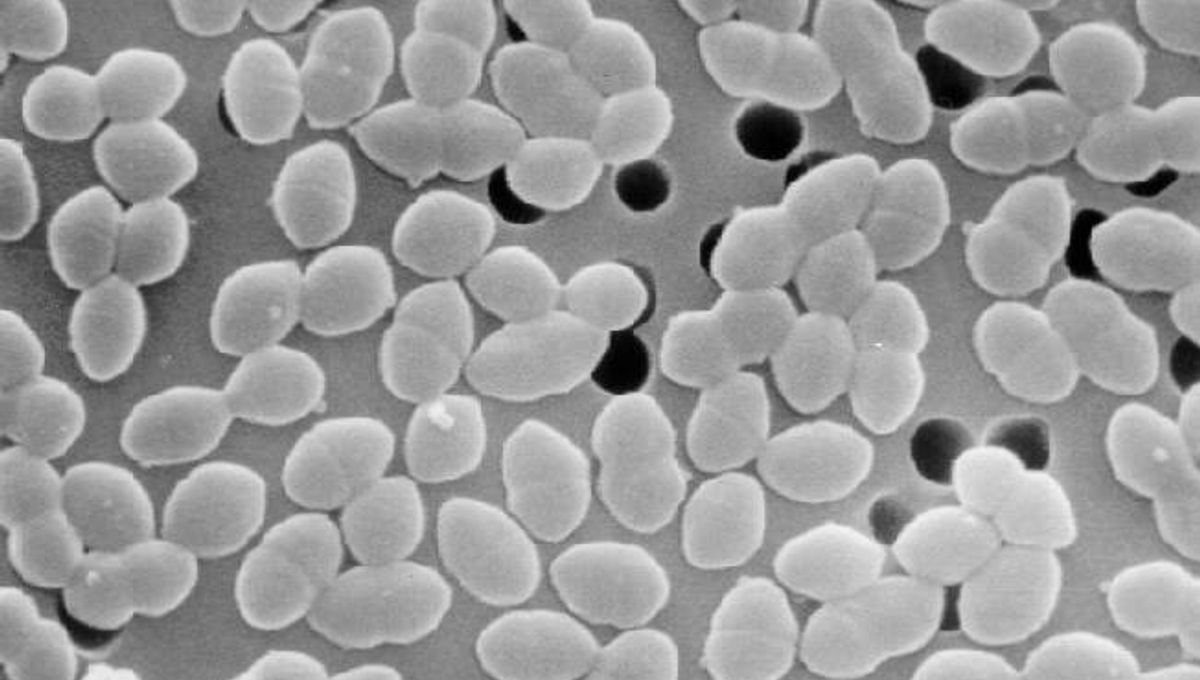
E. faecium is an important cause of hospital-acquired infections. It’s one of a group of bacteria that have been dubbed the ESKAPE pathogens, along with Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species. The World Health Organization has identified these bacteria as serious threats to global public health because they have become resistant to many different antibiotic drugs.
The first-line treatment for E. faecium infections used to be vancomycin. Unfortunately, the spread of resistance genes in bacterial populations around the world has meant that new options are needed to combat vancomycin-resistant E. faecium (VREfm). One of these is a newer antibiotic called daptomycin, which is used off-label to treat VREfm infections as a “last-resort” drug.
But what happens when even your last resort becomes ineffective? As the authors of the new preprint write, “resistance [to daptomycin] has surprisingly and alarmingly been widely reported.” The researchers wanted to investigate how the bacteria could be acquiring resistance so quickly, and they’ve hit on a potential mechanism that we may not have seen coming.
In certain patients with liver disease, another antibiotic called rifaximin – usually a treatment for traveler’s diarrhea – is used to help prevent a serious complication called hepatic encephalopathy. These patients are also more likely to have colonies of VREfm bacteria within their intestinal tracts. The study authors suspected that this use of rifaximin as a prophylactic may somehow be contributing to the rise in daptomycin resistance seen in VREfm bacterial isolates.
The researchers, based in Melbourne, Australia, undertook a series of experiments on bacteria cultured in the lab, as well as in mice, and on bacterial samples collected from patients at a Melbourne hospital who were being treated with rifaximin.
The results showed that VREfm bacteria exposed to rifaximin developed resistance to daptomycin, which was found to be linked to several genetic mutations in the bacterial RpoB gene. Analysis of bacteria isolated from human patients showed that patients receiving rifaximin prophylaxis were significantly more likely to be carriers of daptomycin-resistant VREfm. This was also supported by the results of the mouse experiments.
“Our data suggests the clinical use of rifaximin may be responsible for selecting VREfm isolates harbouring mutations [in RpoB] and therefore, indirectly driving the emergence of daptomycin-resistant VREfm,” conclude the researchers.
“Overall, this research highlights the potentially serious collateral damage that can arise following the introduction of new clinical antibiotic regimens.”
Antibiotic resistance is an ever-growing threat. Efforts to identify and develop new antimicrobial drugs, as well as alternative treatments, are essential as we seek to beat the bugs in this arms race, but it’s also vital that we keep our eyes open to the less obvious ways in which bacteria might be acquiring resistance.
As the study authors say, “These findings […] highlight the negative impact that unanticipated cross-resistance can have on antibiotic stewardship efforts designed to preserve the use of last-resort antibiotics.”
“We advocate for the judicious use of all antibiotics.”
The preprint, which is yet to be peer-reviewed, as available at medRxiv.
Source Link: New Findings May Explain How Bacteria Are Becoming Resistant To A Last-Resort Antibiotic