A new vaccine strategy could spell the end of yearly flu shots, by targeting part of the virus that is much less prone to mutations. So far, it’s worked well in mice and ferrets – could we soon be looking at a human equivalent?
Why do we need to get a flu vaccine every year?
Seasonal flu is responsible for roughly half a million deaths every year. It can be a very serious disease, and spreads easily between people, so vaccines that prime our immune system to recognize proteins on the virus’s surface are our best possible defense.
Unfortunately, the flu virus also has an irritating habit of mutating. A lot. That means we have to constantly update the vaccine to try and keep up. Each year, scientists study the trends from previous flu seasons and tailor the vaccine to the strains of virus they think will be most prevalent.
It’s not a perfect system, and some year’s flu vaccines are better than others, but it does save lives.
What does the flu vaccine target?
The two major surface proteins on an influenza virus are called hemagglutinin and neuraminidase. The different types of these proteins give each strain a shorthand name – you may have heard of H5N1 or H1N1. The H, sometimes abbreviated to HA, is what we’re most interested in.
“On the virus particle, there’s five to 10 times more hemagglutinin than neuraminidase,” said associate professor of molecular genetics and microbiology Nicholas Heaton in a statement. “If we took your blood to see if [you are] likely to be protected from a strain of flu, we’d be measuring what your antibodies do to hemagglutinin as the best metric of what’s likely to happen to you.
“The strongest correlates of protection have to do with hemagglutinin-directed immunity.”
How is this new vaccine approach different?
“A number of groups have gone through and experimentally mutagenized the whole hemagglutinin and asked ‘which areas can change and still allow the hemagglutinin to function?’ And the answer is, you can’t really change the stalk and expect it to continue to function,” Heaton said.
The “head” of the hemagglutinin protein is constantly changing as the virus is locked in an arms race with the human immune system. Heaton and the team came up with a way to get the immune system to shift its focus to a new target instead: the stalk.
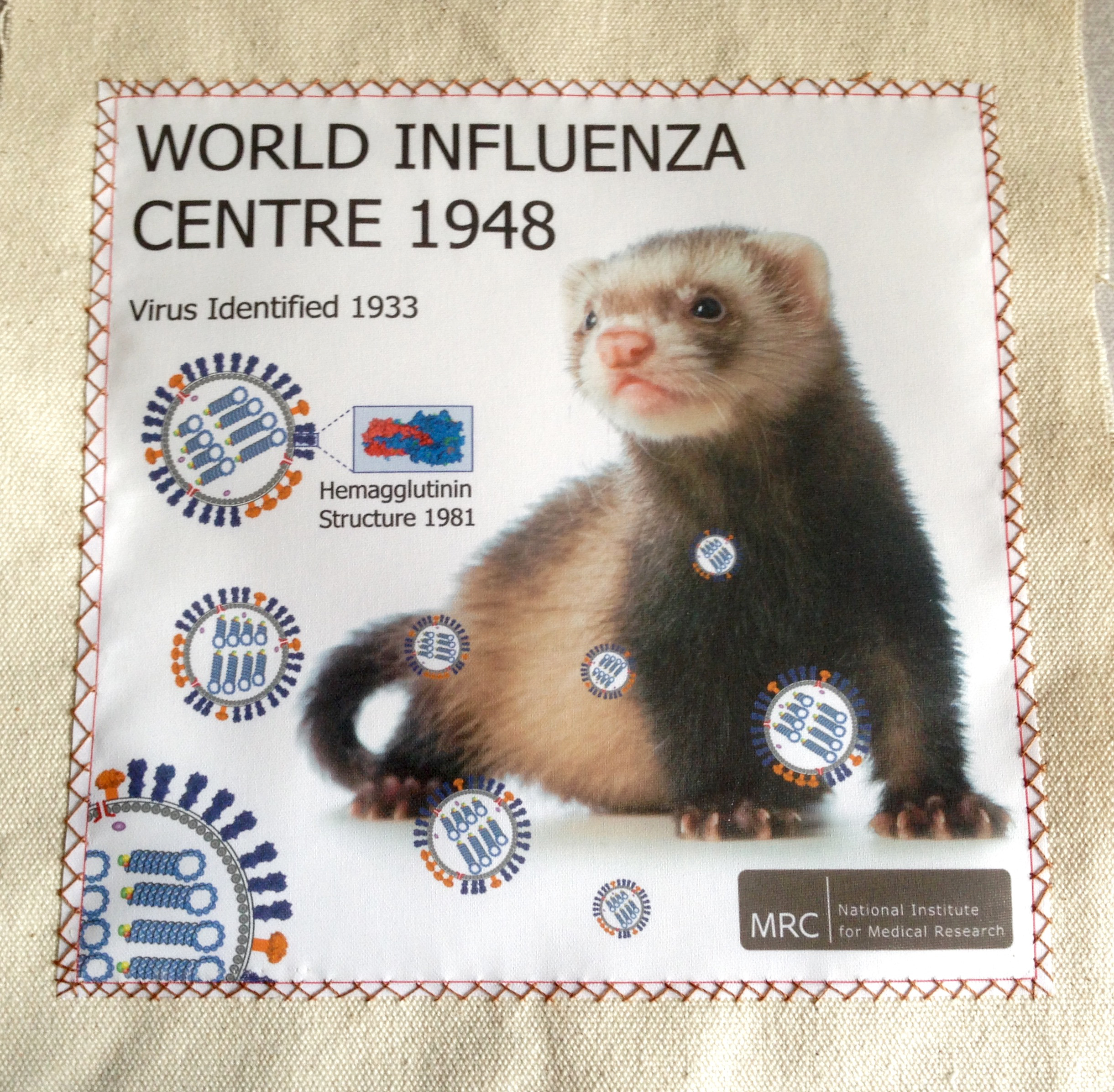
The team generated some 80,000 different variants of hemagglutinin, each with small changes in one section at the top of the head. They mixed a vaccine cocktail of these variants and injected it into mice and ferrets. We don’t see ferrets cropping up in the lab all that often, but they’re a very good model organism for the study of influenza.
Because the hemagglutinin heads being presented to the immune system via the vaccine were all different, whereas the stalks were consistent, this altered the balance of antibodies being generated by the immune system.
Antibodies against the stalk of the protein work differently than those against the head. By creating a vaccine that generates both types of antibodies, Heaton and the team hoped to give the immune system a better chance even if the seasonal strains selected for the vaccine weren’t quite right, or in case a whole new pandemic strain should come along.
“Essentially, the paper says, Yes, we can accomplish that,” said Heaton.
What were the results?
Well, they were pretty impressive. In some of the mouse experiments, 100 percent of the animals avoided illness or death when given a dose of flu that should have been fatal. Across the ferret experiments, the animals given the new vaccine had less severe illness than those given an old-style shot.
However, it’s a little early to get excited. If you want up-to-date protection, you’re going to be scheduling in that annual shot for a good few years yet.
One of the important caveats the authors note in their paper is that the animals they used had no pre-existing immunity to flu. This is not the case for pretty much every human who is not a newborn baby, so it will be important to find out how this approach works in people with a history of previous vaccine or illness.
They also only used one specific type of hemagglutinin, and as we know there are many others out there. More work is needed to completely tease apart the mechanism by which the vaccine prevented serious disease in the animals, and the scientists are also keen to find out whether it can work with fewer than 80,000 different variants.
Ferrets and flu go back a long way – it’s thanks to them that we first discovered the virus in 1933.
All of these questions will hopefully be answered in future studies, and human trials would of course be needed before you could rock up to Walgreens and get your universal flu shot. The results form part of a five-year project – these things are marathons, not sprints.
We might have allowed ourselves to forget, just for a second, what flu can do while our attention was necessarily focused on COVID-19. But with H5N1 avian flu making concerning moves, and this year’s annual season already underway in the Southern Hemisphere, it’s good to think that the universal vaccine we’ve been hoping for is a step closer to fruition.
The study is published in Science Translational Medicine.
Source Link: No More Yearly Flu Shots? Vaccine Mixed From 80,000 Proteins Could Be The Key