An antiviral drug that attacks a SARS-CoV-2 virus protein protects mice against many of the most severe effects of the disease, including some that can linger on. Trials on humans are yet to begin, but the work raises hopes for progress against the ongoing legacy of the pandemic.
Most countries have stopped reporting deaths from COVID, but infection remains common and around 5 percent of those infected will have ongoing symptoms. These can last for years and often drastically affect quality of life. Vaccination has been shown to reduce the risk of long COVID, particularly if kept up to date, but is a long way from eliminating it. Despite causing major reductions in deaths and hospital admissions, taking Paxlovid soon after infection does not appear to reduce long COVID, so something new is needed.
Since early in the pandemic, a team at the Walter and Eliza Hall Institute (WEHI) have thought a drug targeting the coronavirus protein PLpro might be the answer. Even before the pandemic occurred, WEHI’s Professor David Komander had been studying the family of proteins PLpro belongs to in other viruses. Dr Stefanie Bader had started her PhD at WEHI when the pandemic began and told IFLScience she pivoted her research to target the virus, PLpro included.
Bader told IFLScience PLpro is an enzyme the virus uses to replicate and escape one cell to infect others, adding; “It also stops us from fighting the virus.” Consequently, molecules that block or attack PLpro could be helpful in multiple ways.
“Existing drugs had hit several hurdles to be effective in blocking PLpro in cells – our team wanted to see if we could find new ones capable of overcoming these barriers,” said Komander in a statement. “In order to do this, we screened over 400,000 compounds to see if we could uncover novel drug-like molecules that had potential against this protein.”
Work like this is usually slow, but the scale of the crisis has created incentives to speed things up. The team identified a molecule they are currently calling WEHI-P8 and gave it to mice, both before infecting them with SARS-CoV-2 and six and 24 hours afterward. They compared their results with those of mice treated with Paxlovid at the same points.
The mice given WEHI-P8 had lower viral doses and inflammatory responses than those given Paxlovid, let alone those left unprotected. Moreover, these mice had little to none of the signs of damage to the lung and brain associated with long COVID. On the other hand, the results for heart and gut inflammation were much less encouraging.
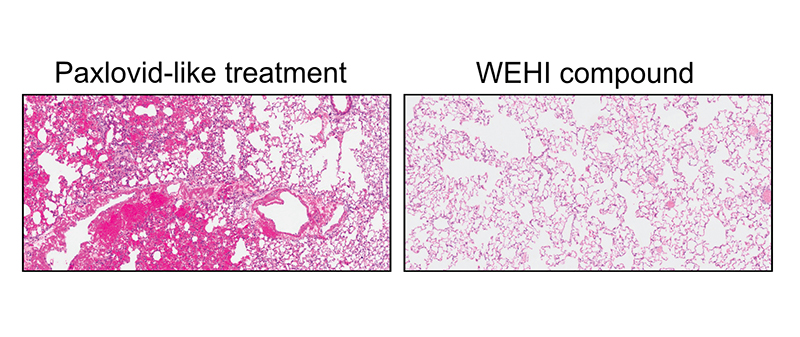
A comparison of lung tissue from mice treated with Paxlovid and WEHI-P8. Dark red indicates damage and inflammation.
Image Credit: WEHI
“Our study has provided the first evidence to prove PLpro is a powerful new drug target for COVID-19 treatments, while also showing its potential ability to treat the virus with unprecedented efficacy,” said Dr Shane Devine.
Paxlovid works on a different pathway from WEHI-P8, targeting the virus’s protein Mpro. Having complementary approaches could be important for acute treatment, since as Devine noted; “The SARS-CoV-2 virus also continues to mutate, meaning it’s only a matter of time until Paxlovid will no longer work. Our findings could lead to a future drug to help close these critical gaps.”
Moreover, Paxlovid interacts with a lot of other medications, preventing many people from taking it safely.
Establishing whether a drug made from WEHI-P8 is safe and effective in humans requires clinical trials. Bader told IFLScience; “As you know, those are very expensive and we’re looking for a partner.”
Only if those trials prove successful will research begin to see if WEHI-P8 can treat long COVID in people who already have it. Even if it doesn’t, with new cases happening every day, prevention could be a major boon to society.
Long COVID has enough similarity to conditions like Chronic Fatigue Syndrome (CFS) that many people have wondered if the cause is the same. Bader said; “Other environmental factors can trigger CFS, and WEHI-P8 won’t work if there is not a viral cause.” However, for many people whose CFS probably was triggered by a virus, there’s a chance it might prove effective.
“We’ve looked for a molecule that doesn’t just inhibit SARS-CoV-2, but other coronaviruses,” Bader told IFLScience. “Viruses change a lot, and if the next pandemic is also a coronavirus, this might work against that as well.”
The study is open access in Nature Communications.
Source Link: Potential Long COVID Drug Works On Mice – Sparking Hope For Much-Needed Treatment