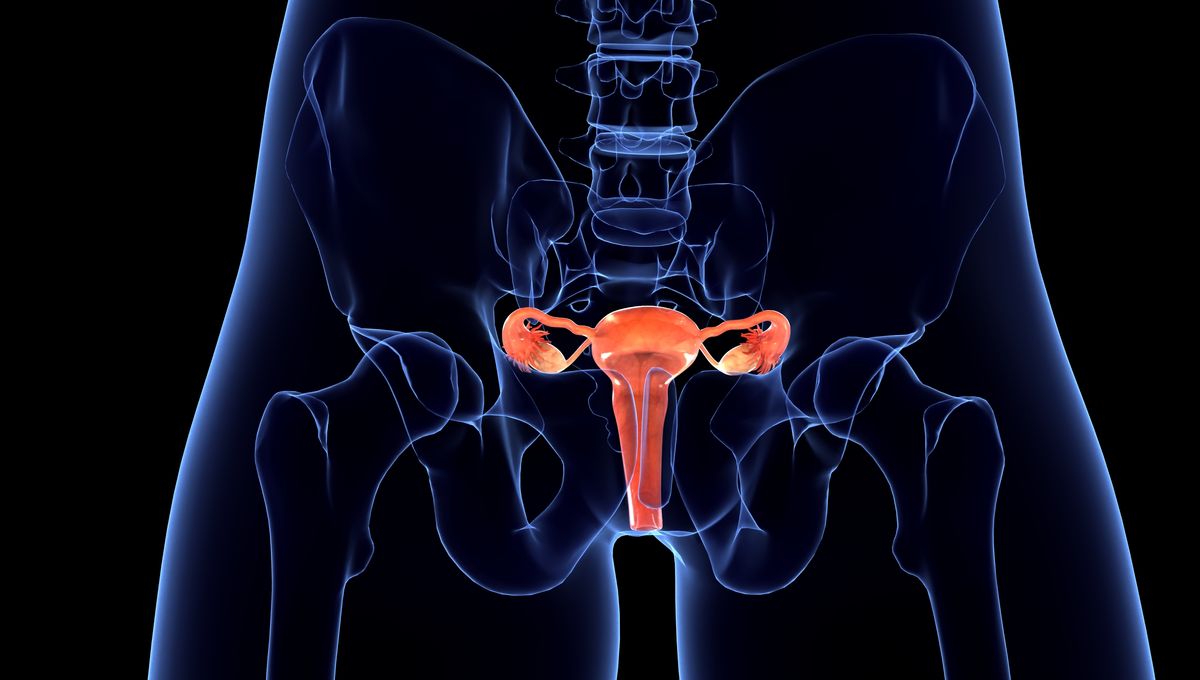
The vagina microbiome: not something that you regularly hear about, but something that plays a vital role in vaginal health and disease. Now, researchers have developed a new technology called the Vagina Chip that will help scientists develop new therapeutic tools.
If you possess a vagina, you may have encountered the uncomfortable condition known as bacterial vaginosis (BV). This occurs when the microbiome of the vagina is disrupted and is the most common vaginal condition between the ages of 15-44.
This disease increases the risk of sexually transmitted infections and the risk of pre-term birth in pregnancy. Fortunately, at the moment, it can be treated with antibiotics – but reoccurrence can happen and leads to severe complications.
There are many bacteria that occupy the vagina, and not all of them are bad. In fact, Lactobacillus species reside in the organ and comprise 70 percent of healthy human vaginal microbiomes. Any disruption of the microbiome can cause disease.
Unfortunately, this area of research is very understudied. This is mainly due to the fact that no preclinical models have been able to replicate the vaginal epithelial microenvironment, as the human vaginal microbiome is a lot different than other common animal models. This lack of preclinical models is essential for experimentation and therapy development.
Well… that is, until now.
“A major stumbling block for that effort was that there were no good preclinical models that could be used to study which therapies can actually treat BV in human tissues. Our team’s project was to create a human Vagina Chip to aid in the development and testing of new therapies for BV,” said co-author Aakanksha Gulati, in a statement.
Researchers at the Wyss Institute at Harvard University have developed and created an in vitro model that features the functional vaginal epithelium: the Vagina Chip, a type of organ chip.
The development of the Vagina Chip required the scientists to seed the top channel of a polymer chip with human vaginal epithelial cells, with human uterine fibroblast cells on the opposite of the permeable membrane. This formed a 3D-like structure of the human vaginal wall. After five days, multiple layers of differentiated human vaginal cells developed.
There have been some successful studies of this technology. For example, when a form of the sex hormone estrogen was introduced, the cells on the chip changed in response, which indicated that it was sensitive to hormones.
The team then went on to test different bacteria on the chip. When a beneficial bacterium like Lactobacillus crispatus is grown on the chips, the epithelial cells remain healthy and produce fewer proinflammatory molecules, consistent with the current theory that these microbes help human vaginas stay healthy.
Researchers also introduced harmful bacteria onto the chips (such as Gardnerella vaginalis) that are associated with BV, which caused the epithelial cells to be damaged, caused the proinflammatory cytokine levels to increase, and the pH to increase. This type of reaction is often seen when there are pathological changes in the human vagina due to an unhealthy microbiome.
“It was very striking that the different microbial species produced such opposite effects on the human vaginal cells, and we were able to observe and measure those effects quite easily using our Vagina Chip,” said co-author Abidemi Junaid. “The success of these studies demonstrate that this model can be used to test different combinations of microbes to help identify the best probiotic treatments for BV and other conditions.”
More work needs to be conducted on this technology, but it is very promising and it could go on to clarify vaginal epithelium-microbiome interaction and also test new therapies.
This study was published in the journal Microbiome.
Source Link: Vagina On A Chip: A Breakthrough For Bacterial Vaginosis Research