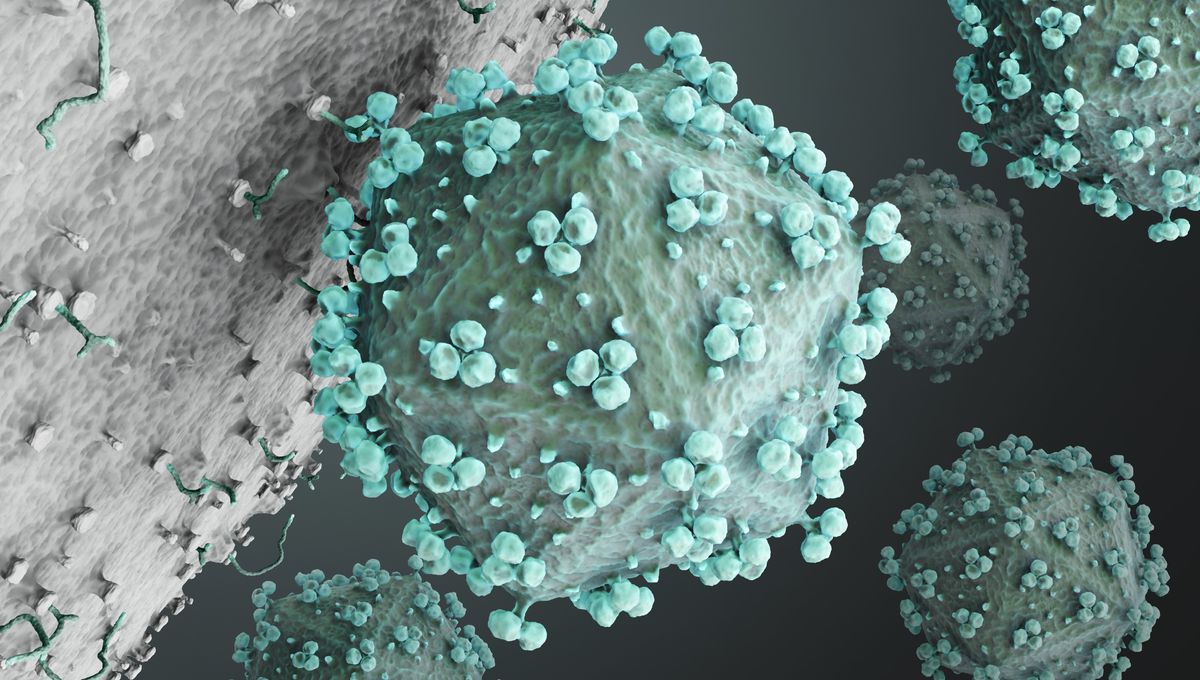
A new study has shown for the first time how human immunodeficiency virus (HIV) binds to T cells. The finding could have implications for new therapies to combat this pernicious disease.
HIV remains a major global public health issue. Since its appearance in the 20th century, the disease has claimed 40.4 million lives and is being transmitted in all countries.
There is no cure or vaccine for the infection, although antiretroviral therapy (ART) helps suppress the virus to undetectable levels in people living with HIV. However, these patients must take medication for the rest of their lives, and for some, the drugs’ effectiveness can fade over time. As such, there is a constant need for new insights to help treat or prevent it.
For some time, scientists have been aware that HIV infects a host by first binding to a cell-surface receptor called CD4. In this new study, researchers used an imaging technique known as cryogenic electron tomography (cryo-ET), to visualize how HIV-1, the most common type of HIV, interacted with virus-like particles (VLP) that carried CD4 receptors. Essentially, this mimicked the way HIV interacts with T cells in nature.
This is the first time this stepwise interaction between proteins of HIV-1 and VLP membranes has been visualized.
“Our study shows the very early stages of how this terrible disease begins and the steps of how it engages with receptors,” to then fuse membranes with T cells, Walther Mothes, PhD, Paul B. Beeson Professor of Medicine at Yale School of Medicine and principal investigator, said in a statement.
Binding process revealed
In this study, Mothes and colleagues used murine leukemia virus (MLV) to produce the VLPs with CD4 receptors. They then observed a mix of HIV-1 and VLPs using cryo-ET to study the interactions occurring on the membrane.
The HIV-1 and VLP gathered in small clusters, which formed rings. HIV-1 was bound to only one CD4 when the membranes were further away, but as they moved closer, HIV-1 bound to a second and then a third CD4.
“We believe these three intermediate steps represent how HIV naturally binds to CD4 on T cells,” Mothes explained.
Previous work had modeled this process, “But they didn’t know if their models existed in nature,” said Mothes. “Our studies on real membranes show that they do.”
Therapeutic implications for HIV and COVID-19
It is hoped that, by targeting the intermediate HIV conformations, new interventions will help prevent HIV infections.
“We have a window where we can specifically target these conformational states with antibodies and drugs,” said Mothes.
An important goal is to prevent HIV, while not interfering with other molecules that are beneficial to cells.
“Imagine HIV viruses as rogue cars running on roads. Current drugs block the lanes to stop virus spread, but they also affect other cars in the traffic,” explained Wenwei Li, PhD, associate research scientist in the Mothes Laboratory and first author of the study. “We are learning what the viruses look like – the color, size, and shape – so that we can specifically target them with drugs, pulling over the viruses without affecting the other cars in the traffic.”
Once a virus binds to a host, the membranes fuse and the virus can proliferate. In future studies, the team hope to examine this fusion in more detail. “There are two steps to infection. We observed step one in this study,” said Li. “And now we are looking for step two.”
The study may also have implications that extend beyond HIV. The team plans to apply its technique to COVID-19 infections, which may help combat this virus as well.
The study is published in Nature.
Source Link: We Now Know How HIV Fuses To Our T Cells, Which Could Impact Future Treatments