What comes to mind when you think about asylums? I bet it involves some large, gothic building on a walled estate. Chances are you are also imagining long sterile corridors, barred windows, white-clothed orderlies, and of course, restrained and straitjacketed patients in various levels of distress. But how accurate is this image?
ADVERTISEMENT GO AD FREE
Asylums have become an archetype for the “darker” side of the history of medicine, and while there are reasons for this, the story is actually more nuanced than many people realize. In many ways, the history of asylums, its good parts and its bad, are all part of the evolving story of how we think about mental illness across time.
The changing face of mental illness
Before discussing the rise of asylums, it is useful to explore how mental illness was understood and treated before these institutions appeared in the 19th century.
For more than 2,000 years, in the West at least, mental illness, like any other illness, was generally (though not exclusively) understood in physical terms related to the body. Of course, Christianity had a heavy influence on all aspects of life throughout the medieval and much of the Early Modern period, which meant that medically trained physicians still believed in demonic possession, religiously inspired mania, and witchcraft as explanations for some mental disorders.
But generally speaking, learned physicians believed that the four humors – special bodily fluids consisting of blood, phlegm, yellow bile, and black bile – regulated a person’s health. If the balance of these humors was incorrect, then the person experienced illness, both physical and mental.
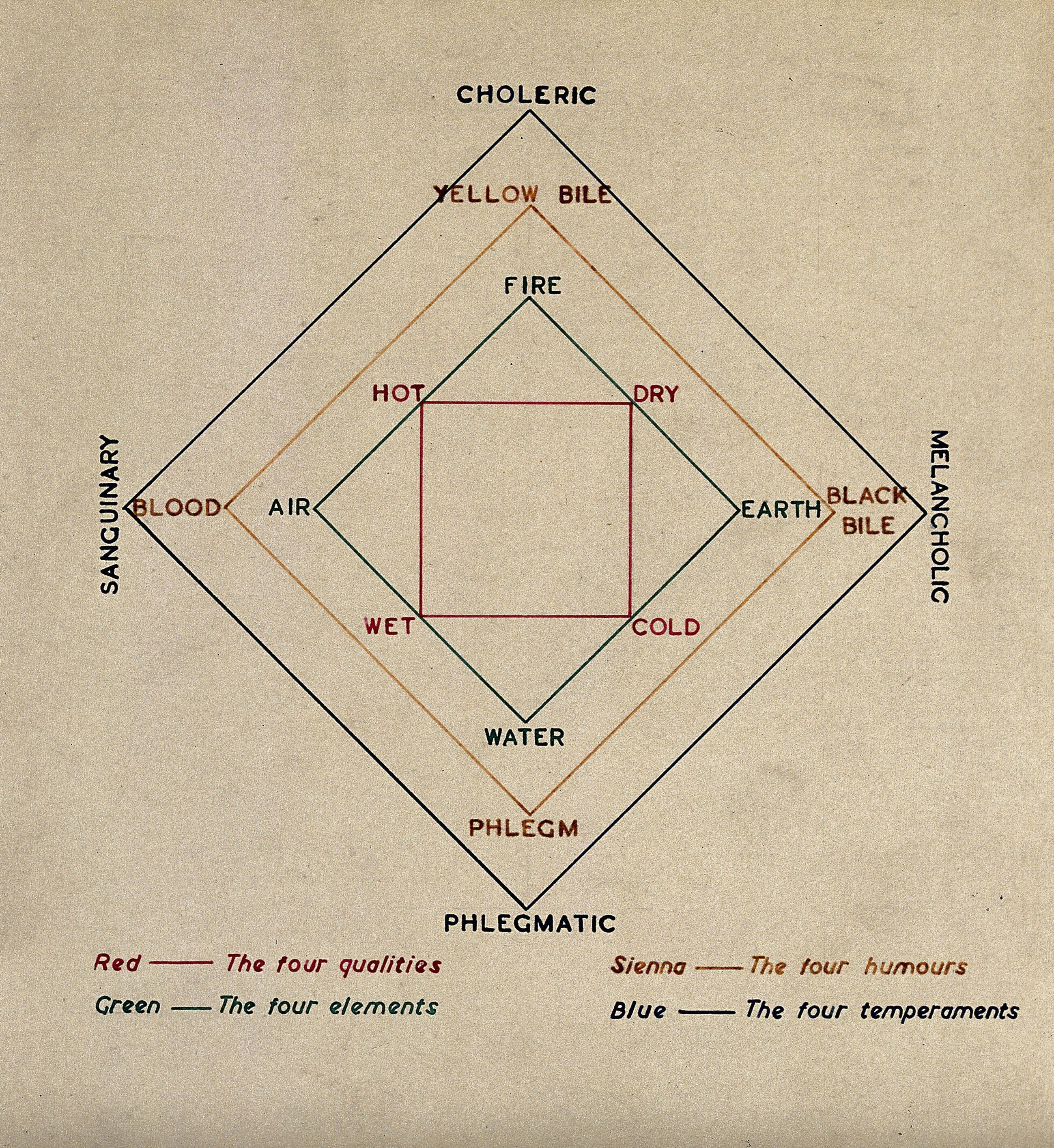
Humoral theory was a sophisticated model in medicine where the four humors were thought to correspond to other aspects of life and the world, including the ages of a person, the elements, and the seasons.
Each person had their own unique mix of these fluids which made up their individual “constitution”, as well as their personality. For instance, the word “melancholic” comes from the idea that a person with a somber or sad temperament probably had a general abundance of black bile in their body. But if someone had too much of this particular humor, then they could develop “melancholia”, a condition marked by persistent sadness, pessimism, and a lack of pleasure in everyday life.
Similarly, if we describe someone as “phlegmatic”, we might regard them as being calm and even-tempered generally, a temperament that was associated with an abundance of phlegm in their body. If, however, a person had too much phlegm, they may become lethargic and apathetic.
ADVERTISEMENT GO AD FREE
Today, we might see both of these cases as signs of depression, but for centuries this was the dominant way to understand changes in a person’s behavior.
In terms of treatments, physicians focused on rebalancing a person’s humors. This often involved adjustments to their lifestyle or diet – certain foods were thought to increase or decrease specific humors. They may also have been bled or offered purgatives in the form of emetics or laxatives – the logic here being that excessive humors could literally be forced out of you. And, of course, physicians had a series of other remedies they could rely on if need be.
But there was no specific place for people with a greater need for support, be it due to illness or disability. Instead, families were responsible for long-term care and those who could not be cared for often became destitute. There were some private institutions in European countries and America by the 1700s that offered to take in residents, but these were often only available to the wealthy and were temporary solutions, while the poor had to rely on support from the local parish. In Catholic contexts, those experiencing mental health issues could seek help from holy shrines, such as the one at Altötting, Bavaria, in the hope of healing miracles. In many instances, these people could end up in charity-funded institutes, workhouses, or prisons.
Confinement and cruelty?
Within these limited custodial spaces, the objective was not to treat or “cure” the inmates, but to merely to keep them “safe”. Those who worked in such places had no medical training and generally just functioned as guards or wardens. Those confined in these spaces could be chained or restrained in other ways, especially if they were deemed violent (to others or to themselves).
ADVERTISEMENT GO AD FREE
Although restraints were common features of such places, the extent of their use varied from location to location. In some cases, patients even requested them as they feared they would otherwise hurt themselves. It is also worth noting that just because these early “asylums” did not have any meaningful ways to treat their inmates, that does not mean they were all places of punishment. In fact, there were asylum-like spaces in places like Juliusspital, at Würzburg, Germany, which appear to have been quite popular with both their patients and their families.
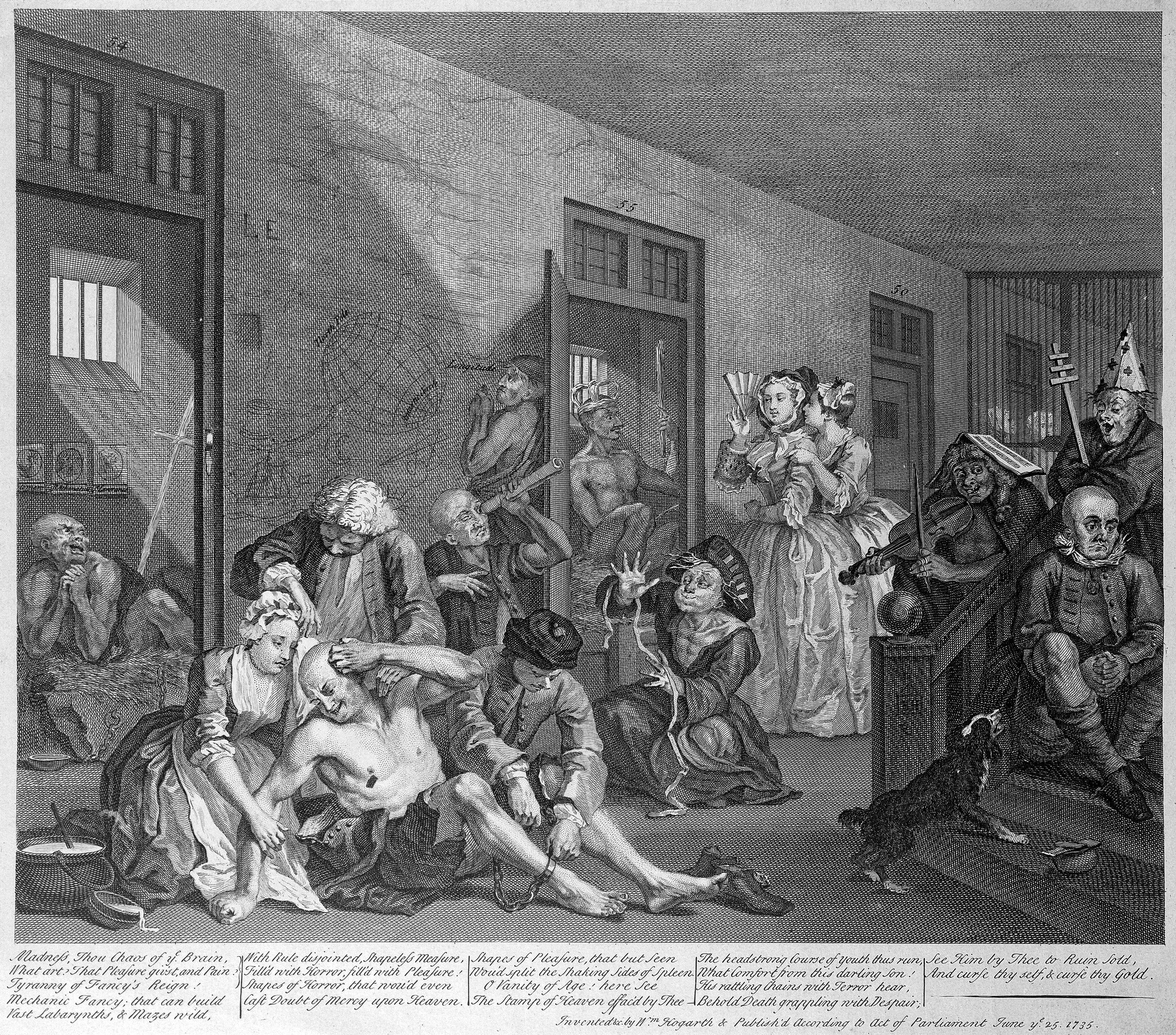
In the early 18th century, William Hogarth produced his series of paintings (and later engravings) showing the decline of an immoral man. The final image depicted a scene in Bedlam hospital, which has now become synonymous with abuses and restraint.
However, because these early forms of “asylum” had no official oversight, no standardization, regulation, or accountability, ultimately, they were vulnerable to abuse.
Bethlem hospital in London, otherwise known as Bedlam, is perhaps the most widely known version of this “house of horrors” concept and is now synonymous with the stereotypical cruelties and excessive mistreatments we associate with such places. But over the last few decades, historians have challenged this caricature. Bedlam, they conclude, has gained a bad rep due to myths, oversimplifications, generalizations, and so on. Its image has also suffered because it has often been compared to later institutes that appeared in the actual age of the asylum.
The rise of the asylums
With the rise of the Enlightenment, a European intellectual movement, in the 17th and 18th centuries, physicians across Europe began to rethink the nature of mental illness. Rather than focusing specifically on the humors, they paid greater attention to psychological processes and the role of the nerves in causing specific disorders. Increasingly, physicians began to specialize in matters of the mind, producing the first “mad doctors” who were now armed with a learned rationale for their specialism.
ADVERTISEMENT GO AD FREE
Most significantly, by the end of the century, the idea that mental illness could be treated, or at least improved, had become more widespread. With it came a more humane approach that saw patients as rational beings.
In 1796, a Quaker called William Tuke established a new kind of asylum known as the York Retreat after the death of a fellow quaker in an asylum. This private mental institute championed the use of “moral treatment” and the minimal use of restraints. Essentially, moral treatment focused on compassion and respect, providing patients with quiet, calm environments that emphasized routine and stability.
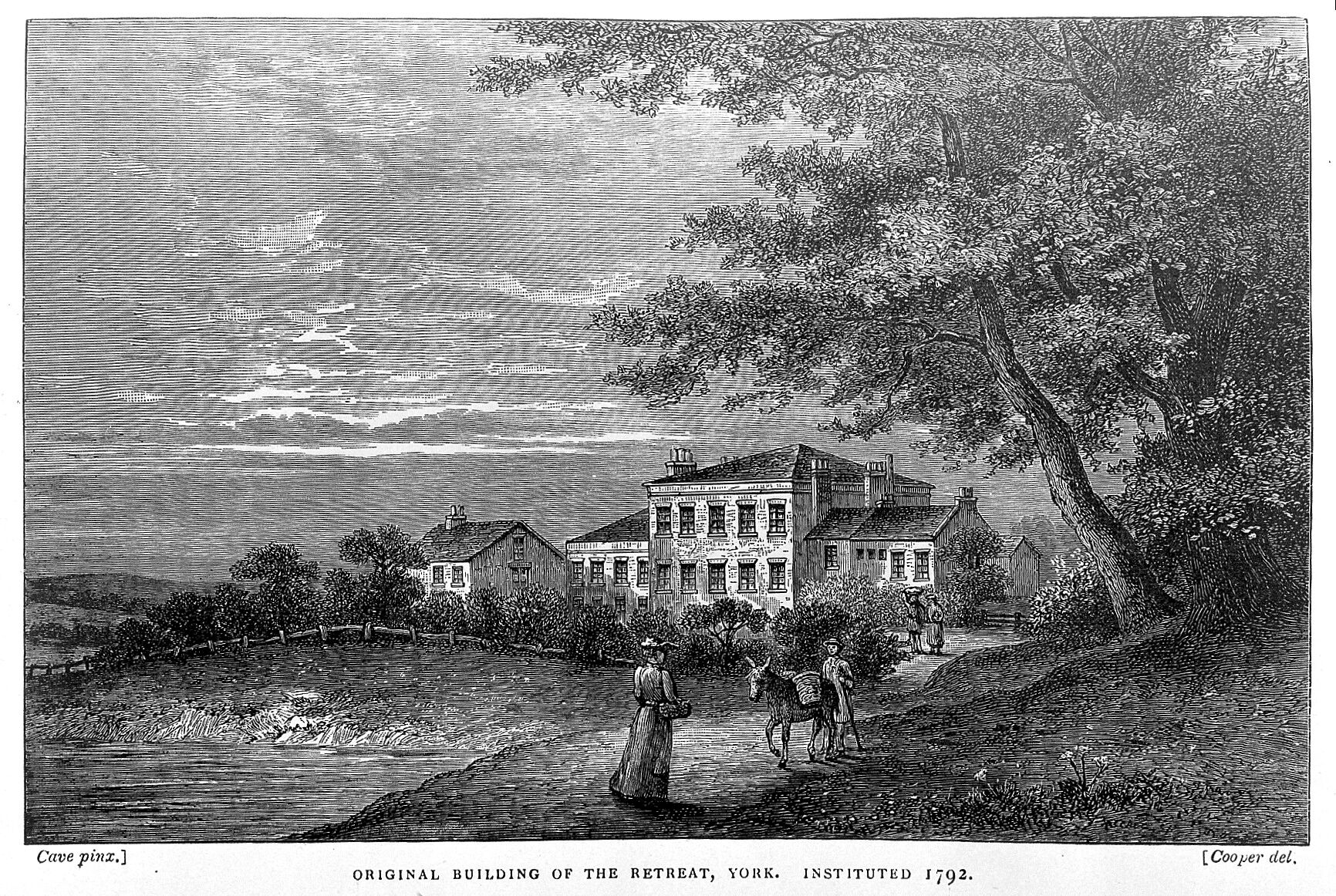
The York Retreat set a new standard for the care of mentally unwell patients that emphasized moral treatment with minimal restraint.
Patients were expected to eat at the table, make conversation, and participate in daily activities and light work, like gardening and crafts. Each patient had a regimen tailored to their needs, and it was enforced through simple rewards or punishments.
Following William, his grandson Samuel Tuke produced his book A Description of the Retreat, which popularized their new treatment methods. It helped set the stage for the rise of Victorian asylums, which sprung up across Britain and the US. Socially progressive and philanthropically-minded people paid for new institutions to be constructed to aid the poor and needy.
ADVERTISEMENT GO AD FREE
However, the success of this innovation was ultimately unsustainable. As the demand for asylums grew throughout the 1800s, the new institutions became increasingly underfunded and often poorly staffed. Rather than “curing” patients, many of those receiving moral treatment simply stayed in care for long periods of time, sometimes their whole lives. This led to overcrowding. Couple that with inexperienced staff and inept or even corrupt management, and it was not long before stories of horrific abuses and negligence emerged.
The fall of the asylums
At the start of the 1900s, moral treatment was largely out of fashion. The gradual rise of medical science in the 19th century had advanced to the point where mental illness was increasingly viewed in biological and, as the 20th century progressed, neurological terms. Now, mental health specialists used standardized and scientific procedures to identify specific symptoms to distinguish different disorders.
For instance, the German psychiatrist Emil Kraepelin (1856-1926) is recognized as a pioneer of the scientific understanding of psychiatry and psychopharmacology, classifying new mental illnesses based on their symptoms and causes, which led to the diagnosis of things like “dementia praecox” (what we would call schizophrenia today) and “manic-depression” (now understood as bipolar disorder).
What did this mean for asylum patients? Well, the new emphasis on medical causes and symptomology led to increasingly specific invasive therapies. For instance, in the late 1920s, the use of insulin shock was developed by the Australian-American psychiatrist Manfred Sakel, to treat schizophrenia. This involved putting patients into a coma on a daily basis – the treatment program could last for weeks – by injecting them with large doses of insulin. The belief underpinning it was that, by inducing extreme hypoglycemia, the patient’s brain functions would essentially “reset”.
ADVERTISEMENT GO AD FREE
At a similar time, electroconvulsive therapy (ECT) was also introduced to treat severe mental illnesses, such as depression and schizophrenia. This notorious treatment involves electrically inducing seizures in anesthetized patients. As with insulin shock, the belief was that these seizures would disrupt abnormal brain activity and reboot normal functions. It is worth noting that despite its controversial history, ECT is still used today for some conditions but its applications have changed since the 1930s.
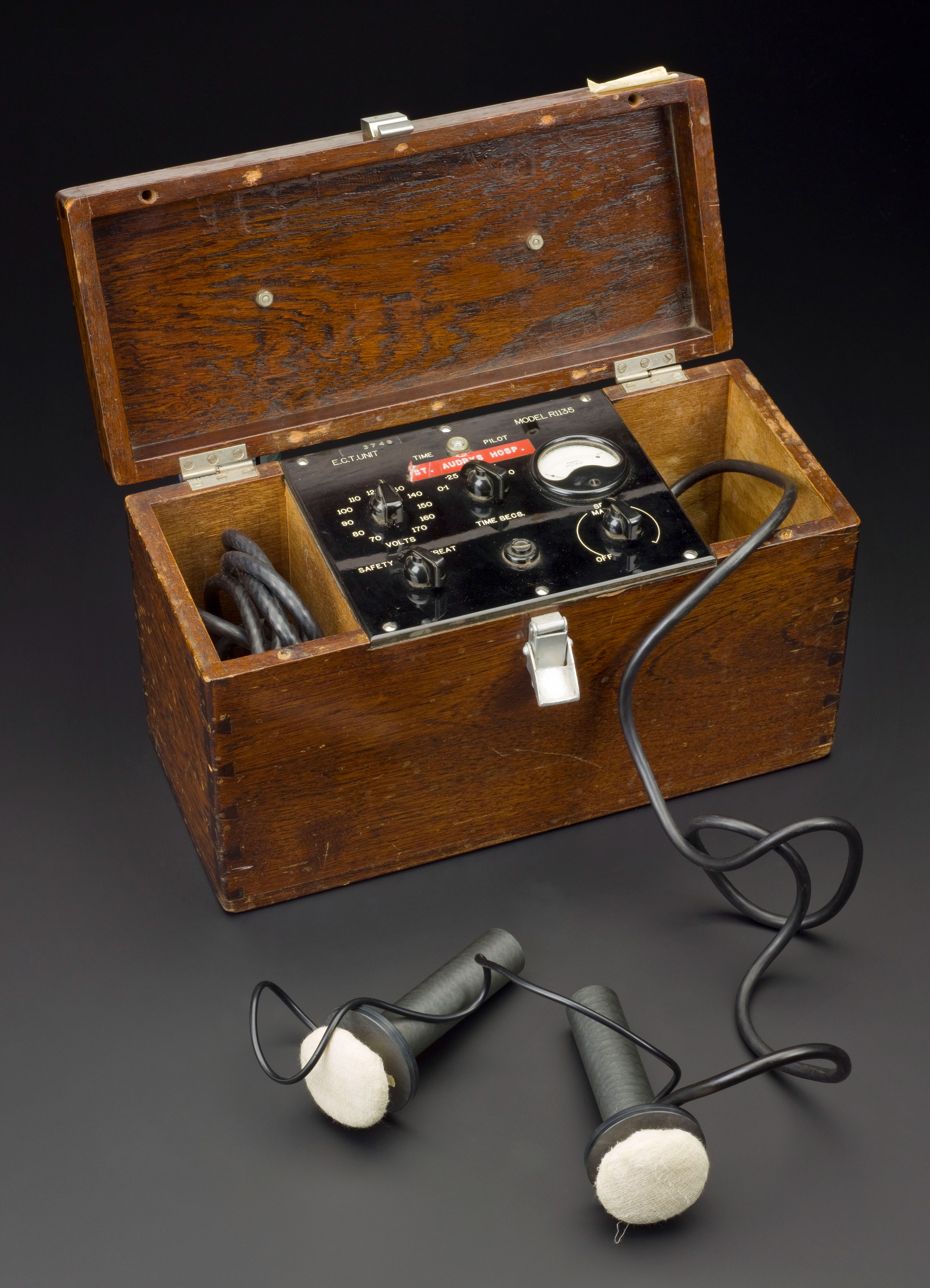
This is an example of an electroconvulsive therapy machine that is currently housed at the Science Museum in London.
Another innovation that has become synonymous with the horror of asylums was the introduction of lobotomies as a form of psychosurgery. This technique operated on the belief that mental illnesses were caused by dysfunctional neural pathways. By cutting the connections between the frontal lobe and other parts of the brain, it was argued, abnormal thought patterns could be disrupted, therefore alleviating psychiatric symptoms. However, those who underwent this intervention often experienced dramatic personality changes.
But the most significant development in patient care came in the 1950s and 1960s, with significant advances in psychopharmaceuticals, especially the development of lithium, chlorpromazine (Thorazine), trifluoperazine (Stelazine), and diazepam (Valium), among others.
The introduction of these drugs revolutionized the treatment of mental illness as they managed patients’ symptoms more effectively than the intense interventions mentioned above. At the same time, this new approach to treatment effectively allowed for the deinstitutionalization of patients, a move that was embraced by many as the asylums became more of a financial burden. Civil rights movements had been advocating for the rights of the mentally ill, so the move away from the crumbling, underfunded asylums was seen as a moral victory that pushed for more humane treatment options.
ADVERTISEMENT GO AD FREE
Over the following decades, government policies came to favor community care options that were cheaper to fund. As such, the last asylums fell into further financial decline, becoming drab, outdated institutes before they were abandoned altogether or repurposed for other healthcare needs. But while community care may have seemed like a cheaper alternative, models like America’s Medicaid and Medicare, introduced in the 1960s, only offered short-term support.
Even today, many community mental healthcare programs are drastically underfunded, poorly staffed, and fragmented in terms of the services they provide. Regrettably, many former asylum patients slipped through the net and, rather than receiving continued support, have ended up homeless or in prison. As such, there is still a long way to go to strike an effective balance between the services offered by asylums and those at the heart of current approaches to mental health.
Source Link: Were Asylums As Bad As People Think? The Rise And Fall Of The So-Called “Madhouse”