A new report describes a case of a rare neurological condition called sixteen syndrome, one of a family of disorders with similarly numerical names. The condition is so unusual that only a handful of cases have appeared in the medical literature before – and, in this particular case, the patient’s symptoms could also help medics answer some long-held questions about a widely used class of drugs.
Sixteen syndrome is one of several conditions given the collective name of “one-and-a-half syndrome disorders”. The most commonly reported of these is eight-and-a-half syndrome; other examples include fifteen-and-a-half syndrome and twenty-four-and-a-half syndrome. While these names may seem a bit of a mouthful, there’s actually a really logical explanation behind them.
What all of these disorders have in common is that they affect structures in the brain called the pontine nuclei. Located in a part of the brainstem called the pons, these nuclei play an important role in controlling movement, carrying information from the cerebral cortex. Damage to the nuclei can cause a wide range of different symptoms, so clinicians categorize these disorders by numbering them, according to exactly where the damaged part of the brain is in relation to other structures.
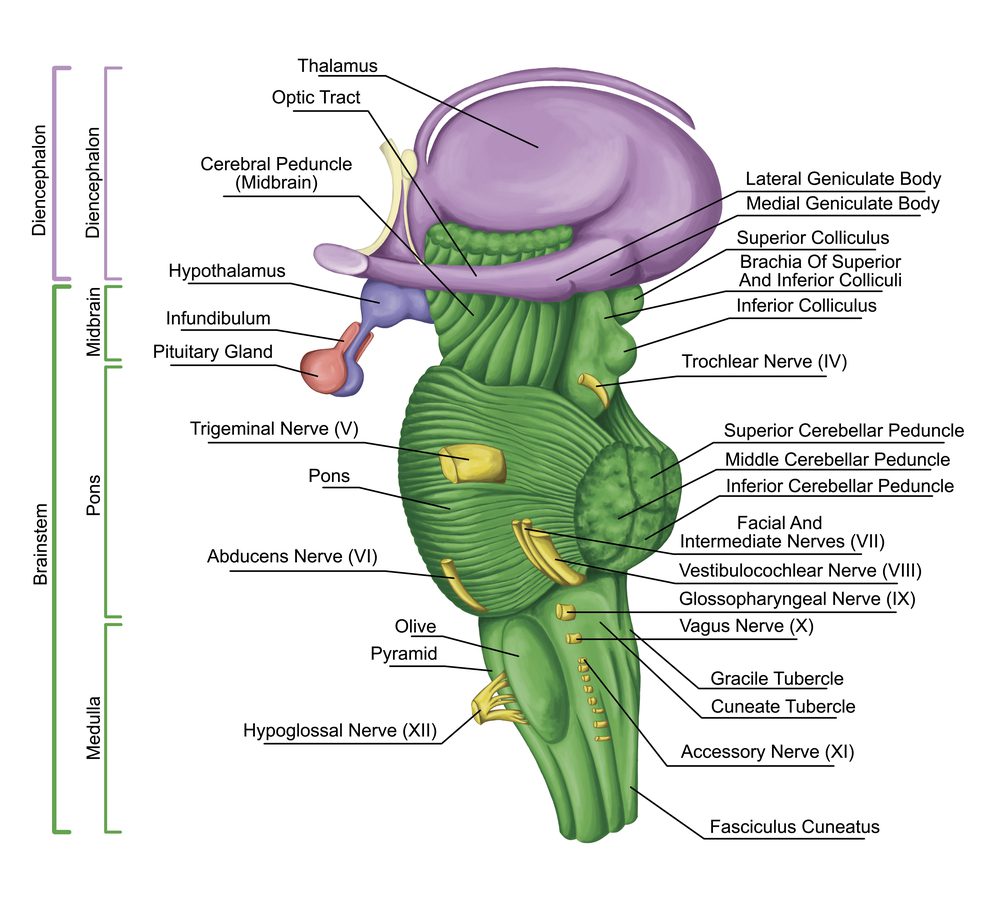
This diagram shows how damage to the pons could easily affect important nearby nerves, such as the facial nerves, leading to the symptoms of sixteen syndrome. Image credit: stihii/Shutterstock.com
Sixteen syndrome causes defects in horizontal eye movement and also affects the facial nerves. The patient in the recent case study had been experiencing headaches, before she developed some worrying changes to her vision: “The following day my eyesight was strange, best described as double-vision. I watched my daughter’s dance team performing and what was usually a troupe of 12 girls looked more like 20!”
Over the next few days, the patient’s eyesight worsened, and the muscles in her face began to seize up. Magnetic resonance imaging (MRI) scans showed evidence of demyelination – depletion of the insulating myelin sheath that sits around nerve cells – in the patient’s brain, consistent with a diagnosis of multiple sclerosis (MS). Other cases of sixteen syndrome, as well as different one-and-a-half syndromes, have been described in patients with MS – it’s all to do with exactly where the demyelination happens in the brainstem.
Although the patient began to experience some relief from her symptoms after treatment in hospital, receiving a diagnosis of MS would be a life-changing thing for anyone to face. However, there was something else in this patient’s history that meant that the case was not quite as simple as it first appeared.
Several years earlier, the patient had been diagnosed with an autoimmune disease called ankylosing spondylitis. There is no cure for the disease, but the debilitating stiffness, back pain, joint and tendon inflammation, and fatigue it causes can be managed with treatments that seek to delay its progression. The patient in this case was being treated with a class of drugs called tumor necrosis factor alpha (TNF-α) inhibitors.
TNF-α is a vital part of the immune system, but in autoimmune conditions, the immune system goes haywire and starts attacking parts of the body. TNF-α inhibitors, such as adalimumab and etanercept, are commonly used to treat diseases like ankylosing spondylitis, Crohn’s disease, and rheumatoid arthritis. Like all medications, TNF-α inhibitors can cause side effects. For a long time, there has been a question mark over whether these drugs might be a possible cause of demyelination in the brain.
Back to our patient. She had been taking adalimumab, which she described as a “game-changer” for her ankylosing spondylitis. However, was it possible that the very drug that had helped her so much was now causing an MS-like pathology in her brain?
The clinicians handling the case concluded that they simply cannot be sure, although it is possible: “It is plausible in our case that the demyelination may be related to our patient’s use of a TNF-alpha inhibitor, despite the fact that her symptom onset was greater than 12 months after commencement of adalimumab.”
Research into the possible side effects of TNF-α inhibitors will continue – in the meantime, if you’ve been prescribed these drugs it’s important that you don’t stop taking them, but talk to your doctor if you have any concerns.
We may also have some more numbers to add to the list of one-and-a-half syndromes before long. Although these conditions are rare, recognizing them can help doctors unlock a piece of a tricky medical puzzle. And, at least in this case, the patient’s report ends on an optimistic note.
“Some questions will never be answered, but I will head into the future with a supportive medical team and a great circle of friends and family by my side.”
The paper is published in BMJ Case Reports.
The content of this article is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of qualified health providers with questions you may have regarding medical conditions.
Source Link: What Is Sixteen Syndrome?