It’s the longest nerve in the autonomic nervous system, stretching from the brain stem all the way down through the chest, neck, and abdomen. Its approximately 160,000 fibers connect it to multiple key organ systems, and it’s responsible for regulating many of the processes that keep us alive. It’s called the vagus nerve, and right now it’s seriously hot property in the wellness world.
There’s been a lot of buzz around the idea of stimulating the vagus nerve to relieve all sorts of health issues, but how much truth is there in it? We take a look at what makes the vagus nerve so important.
What does the vagus nerve do?
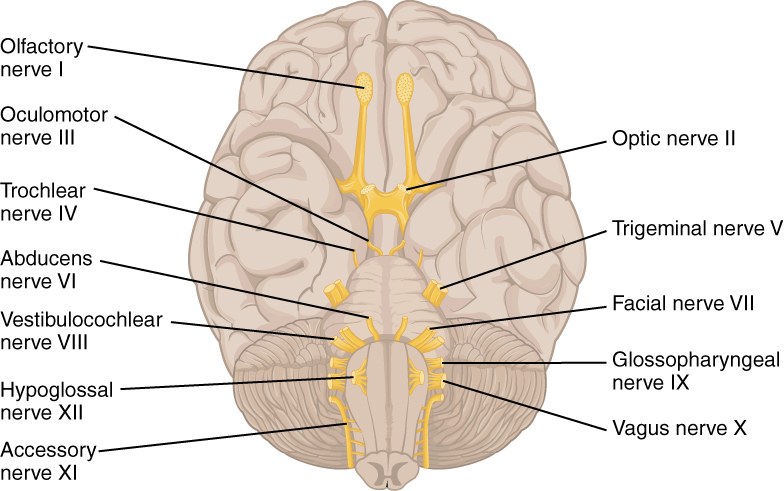
The vagus nerve is actually a pair of nerves, one left and one right, but it’s usually referred to as one single entity. It’s the 10th of the 12 cranial nerve pairs that provide electrical conductivity between the brain and all parts of the head and upper body – these include the olfactory nerve, which gives us our sense of smell, and the optic nerve, which controls sight.
The 12 cranial nerves.
The vagus nerve is the grandaddy of cranial nerves. It’s by far the longest and branches out into all the critical organ systems in the neck, torso, and abdomen. In fact the very word “vagus” comes from the Latin for “wandering”, illustrating just how many different bodily functions rely on it in some way.
The vagus nerve also makes up an estimated 75 percent of the parasympathetic nervous system, the subsystem that controls processes that we think of as “automatic”, such as the passage of food through the digestive system and the rhythm of the heart. The parasympathetic nervous system takes over when we’re in the so-called “rest and digest” phase, while the counterpart sympathetic nervous system controls the “fight or flight” response to stress and danger.
And if you’ve ever passed out from shock or standing still for too long, you can thank your vagus nerve for that too – occasional fainting due to a drop in blood pressure is also known as vasovagal syncope.
Because it has its noodly fingers in so many pies, so to speak, the vagus nerve and its potential dysfunction have been implicated in lots of health conditions. Many a wellness blogger has touted the supposed benefits of vagus nerve stimulation – but is there any science to back this up?
Ice baths, humming, and vagal tone
A quick search on TikTok is all you need to confirm the buzz around “resetting” or “hacking” your vagus nerve as a gateway to wellness.
One name that has become inextricably linked with all this is that of Wim Hof, the Dutch “Iceman” famed for his penchant for extremely cold environments. Hof claims to have developed a breathing technique that allows him to “voluntarily influence his autonomic nervous system”, according to his own website.
Hof’s ability to withstand the cold and promotion of the benefits of ice baths have inspired a BBC TV series and a lot of interest from within the scientific community, but also a fair bit of criticism.
One small study into the potential anti-inflammatory effects of following Hof’s methods found that, though the participants did experience decreased inflammation, they also had high levels of adrenaline, more often associated with the sympathetic, fight or flight, nervous system. “This is pretty much the opposite of what you’d expect if Hof’s techniques were working through the vagus nerve,” study author Matthijs Kox told the Guardian.
If you don’t fancy ice-cold immersion, other methods that appear in videos and how-to guides about the vagus nerve include eye movements, neck exercises, and humming. The idea is that improving the tone of the vagus nerve through regular stimulation makes it better able to respond to daily stressors, helping with anxiety and overall well-being.
Proponents of these techniques say people with better vagal tone have more variable heart rates, demonstrating how their body is able to react in an agile way to its changing environment. However, critics would say that these techniques likely make people feel better simply because they are relaxing, rather than them having a significant effect on the vagus nerve itself.
Medical applications of vagus nerve stimulation
There are a number of legitimate medical applications for vagus nerve stimulation, and more research is happening all the time. Unlike the “natural” methods, however, these use electricity to directly stimulate the nerve fibers.
In 1997, the US Food and Drug Administration (FDA) approved the treatment for patients over the age of 12 with treatment-resistant epilepsy, and in 1999 as an adjunctive treatment for adults with major depressive disorder.
There have been some promising studies suggesting it could be beneficial in some patients with inflammatory bowel disease, due to the link between the vagus nerve and the immune system via the spleen. Other studies have looked at its potential in treating pain.
At present, most such therapies rely on a stimulation device implanted into the patient’s neck. There’s a precedent for this type of treatment – it’s not dissimilar to deep brain stimulation – but there will always be a desire to look for a noninvasive method to try to limit side effects as much as possible.
An X-ray image showing an implanted vagus nerve stimulator.
A study in 2022 was the first to show that noninvasive vagus nerve stimulation could strengthen gut-brain communication. The study used electrical stimulation delivered via the skin near the ear, and the increased coupling between the brain and stomach was confirmed using brain imaging and electrogastrogram recordings. The paper concluded that the work could open the door to new treatments for digestive conditions and eating disorders.
There are also trials ongoing for similar noninvasive stimulation methods in patients with conditions as diverse as postural orthostatic tachycardia syndrome (POTS) and Sjögren’s syndrome, and a recently published pilot study showed promise for motor recovery in patients who have had a stroke.
Like many topics that gain traction in the wellness world, there’s a grain of truth to the idea that dysfunction of the vagus nerve could be contributing to poor health in some people. For those people, medical research will continue to look at newer and better ways of stimulating the vagus nerve to hopefully relieve their symptoms.
But for the rest of us? We wouldn’t necessarily recommend hurling yourself into the nearest ice bath, but practices like meditation and yoga – while the jury’s out on how much they impact the vagus nerve itself – can certainly be healthy additions to your lifestyle. Meanwhile, research will continue to uncover more about the many and varied functions of the body’s autonomic “superhighway”.
All “explainer” articles are confirmed by fact checkers to be correct at time of publishing. Text, images, and links may be edited, removed, or added to at a later date to keep information current.
The content of this article is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of qualified health providers with questions you may have regarding medical conditions.
Source Link: Why Is The Vagus Nerve So Important?