The bacterium Chlamydia pneumoniae can infect the central nervous system. In mice, it has been found to trigger responses matching those seen in people with Alzheimer’s disease- notably, the build up of plaques made of the protein amyloid beta, which are the main way Alzheimer’s is distinguished from other forms of dementia.
Although Chlamydia is usually thought of in association with genital infections, C. trachomatis is just one species of a large bacterial genus, whose species infect many animals in different and painful places. As its name suggests, C. pneumoniae is primarily a respiratory tract infection, including the nose, but the possibility it can get from there to the brain is what really has scientists worried.
Professor James St John of Australia’s Griffith University infected mice with C. pneumoniae and discovered that the mouse nose is a key pathway to infection of the brain.
“We’re the first to show that Chlamydia pneumoniae can go directly up the nose and into the brain where it can set off pathologies that look like Alzheimer’s disease,” St John said in a statement. “We saw this happen in a mouse model, and the evidence is potentially scary for humans as well.”
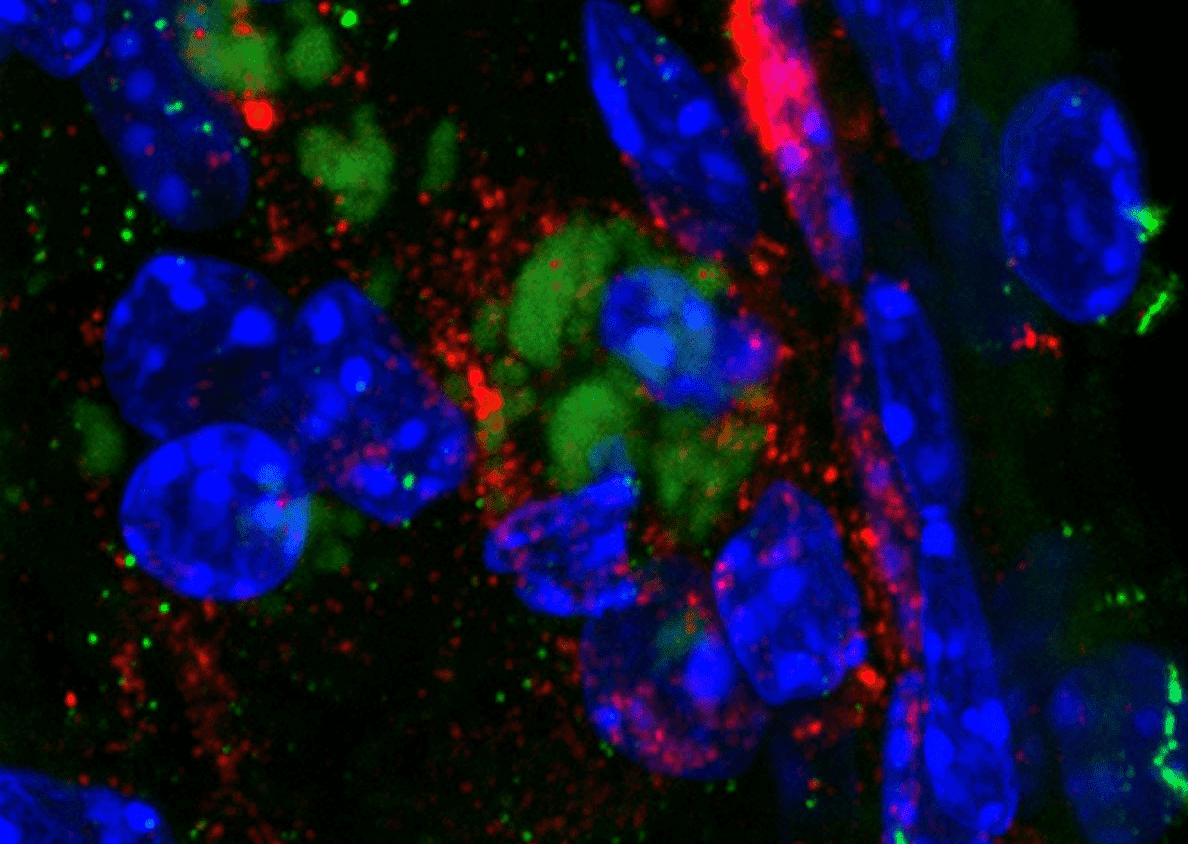
Bacterium Chlamydia pneumoniae (green) inside the brain of a mouse, and surrounded with beta amyloid peptide, the identifying sign of Alzheimer’s disease (red). The frequent association of the bacterium with Alzheimer’s has been known for a long time, but how it gets in has been the question. Image credit: Griffith University
St. John acknowledges that the work needs human replication, although it may be difficult to conduct studies in the same way. Soccer players may be willing to sign up for an increased risk of dementia in return for fun, fame and potential riches; few find respiratory diseases so enticing. However, the fact C. pneumoniae DNA has been found in post-mortems of the brains of 90 percent of late-onset dementia patients, but only a handful of people who died of other causes, is unlikely to be coincidental.
Meanwhile the mouse data is alarming, with the bacterium spreading from their noses to the olfactory nerves and brain within 72 hours. Pathways associated with Alzheimer’s were dysregulated within 7-28 days after the bacterium’s introduction.
If humans are similar, we rely on the inner lining of the nose to keep bacteria from spreading up the olfactory nerve to the brain. Damage to this layer in the mice increased bacterial spread to the peripheral nerves and olfactory bulb. “Picking your nose and plucking the hairs from your nose are not a good idea,” St John said. “We don’t want to damage the inside of our nose and picking and plucking can do that.”
Bad news for aye-ayes, recently discovered to put their freakishly long fingers further up their noses than any COVID-19 swab.
Alzheimer’s isn’t the only reason to worry about C. pneumoniae. Although it accounts for only 5-20 percent of cases of pneumonia, it has been associated with asthma and there is evidence it raises the risk of lung cancer. St John’s work is not the first time it has been linked, albeit tentatively, to diseases of the central nervous system. The presence of C. pneumoniae in the cerebrospinal fluid of patients with multiple sclerosis at much higher rates than in healthy controls indicates the possibility it could be the trigger that causes the immune system to attack the nervous system.
Social sanctions against nose-picking may have a good underlying reason, but disapproval of visible nasal hair may be less evolutionarily beneficial.
The study is published in Scientific Reports.
Source Link: Picking Noses Or Pulling Nasal Hairs Could Raise Alzheimer’s Risk